Deciding Between In-sourcing VS Outsourcing Credentialing Services? Start Here
Deciding Between In-sourcing VS Outsourcing Credentialing Services? Start Here
As visionary leaders, innovators, and healers, you already know that a smooth provider credentialing and payor enrollment process is the key to a healthy revenue cycle. And you also know there are exactly 2 choices when it comes to ensuring providers are properly credentialed and enrolled with each of your payors: In-source or Outsource.
At InteCare, we get it. The daily grind of running your health care center leaves very little time for changing methods of tedious administrative tasks like provider credentialing and payor enrollment.
PLUS, A lot of healthcare leaders put off outsourcing credentialing services since they think it will cost more and give them less control.
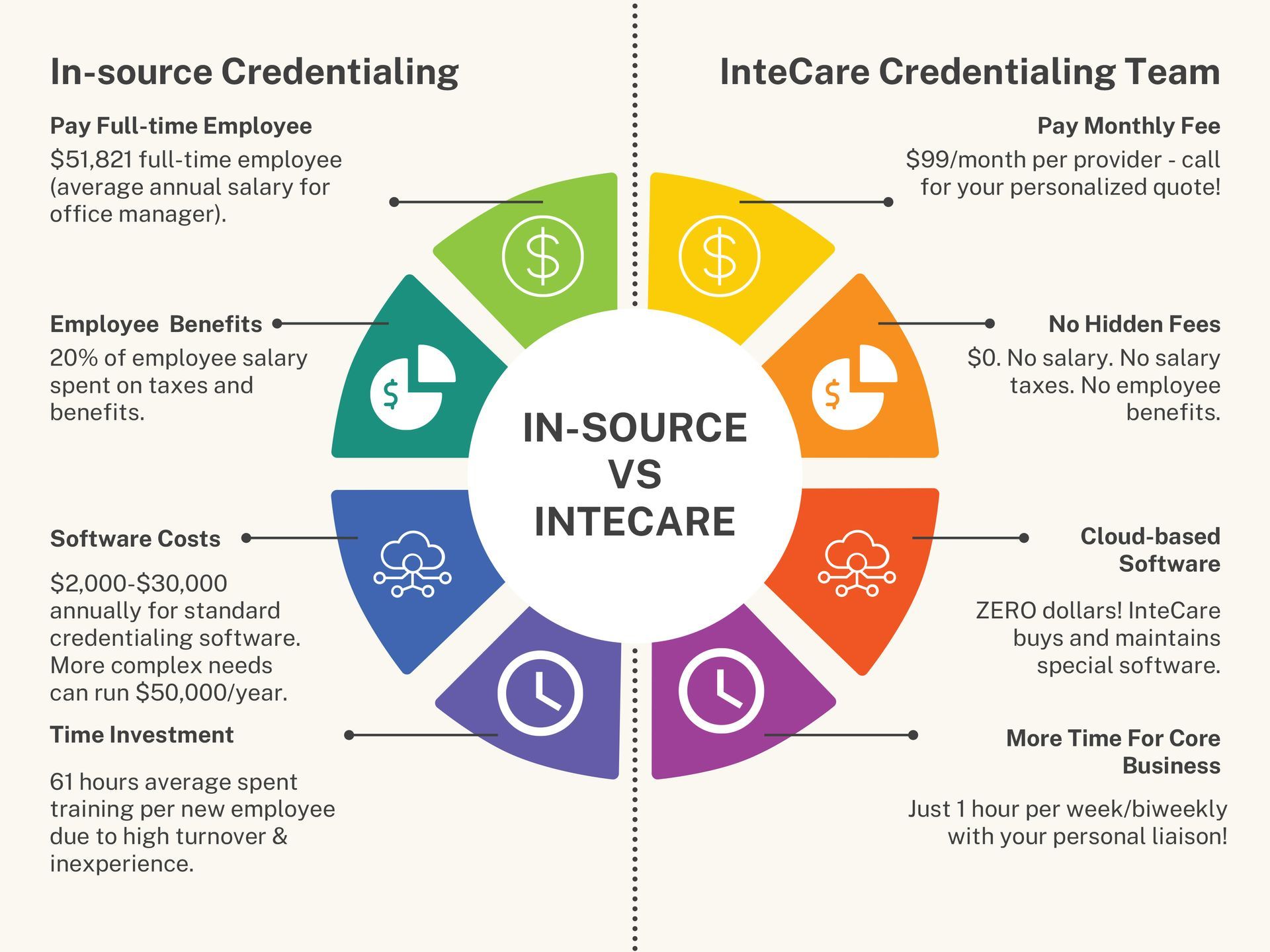
Here is a simple cost comparison to help you crunch the numbers and see how outsourcing credentialing services can give you a solid foundation to confidently run your healthcare center.
Still unsure? Let’s take a deeper look:
In-sourcing with a full-time employee
- Huge Overhead: You’ll have to pay employee benefits, salary (+ salary taxes), the upfront cost of software, monthly software fees, and IT costs.
- High Turnover: The reality is that healthcare (like every other industry today) is struggling to keep employees. You’ll face the hidden costs of time spent hiring and training new employees.
- Competing Demands: Your full-time employee will likely wear many hats in the office and have other responsibilities in addition to provider credentialing and payor enrollment. Without specialized knowledge or experience, there is a greater risk of mistakes.
Outsourcing to a team of credentialing experts
- Cost-effective: You’ll have a monthly fee that charges only for providers on staff that month. No employee benefits. No salary. No software costs.
- Extensive Experience: You’ll have access to a large pool of talented provider credentialing and payor enrollment professionals across the nation. PLUS you’ll benefit from their established relationships with payors.
- Full-time Team: With an entire team dedicated full-time to provider credentialing and payor enrollment, regular meetings, and your own assigned liaison, you’ll cut out costs and streamline internal operations with credentialing done right and on time!

Even if you decide to stay in-house, there is a limited knowledge pool of complex regulations and different states. It is HARD (read nearly impossible) to find staff in rural areas with credentialing experience! When you grow and expand into new territories, your full-time employee will have to learn new, unfamiliar states, wasting time and risking denials.
Now if you HIRE experts…And give yourself permission to hand off this overwhelming administrative burden…The truth is, you will maximize your return and experience higher profit margins so you can confidently run your healthcare center while boosting patient and provider satisfaction!
Ready to move from FRUSTRATED to CONFIDENT?
At InteCare, we help healthcare organizations streamline their provider credentialing and payor enrollment process to better serve their community. Together we’ll shatter barriers to care and drive better outcomes for all. All you need to do is schedule a consultation
here.